The most interesting part of developing predicting models in health care is their application to clinical practice. Thanks to the H2020 European Project, the Bounce Consortium was able to develop models that can predict long-term breast cancer patients’ resilience since the very beginning of the oncological treatment. Besides the identification of patients at high risk for developing long-term poor resilience, the Bounce Decision Support Tool (DST) guides health care professionals toward optimal psychological interventions by identifying the factors that are most likely to promote or, conversely, thwart resilience. The identification of resilience predictors and congruent personalized psychological interventions is crucial to support oncological treatments in ensuring satisfactory patient wellbeing in the long term.
In this perspective, an intervention study has been designed and received approval from the IEO Ethics Committee to test the Bounce Decision Support Tool on 60 breast cancer patients, aged 40 to 70 years. More specifically, before starting the systemic oncological treatments, just after the first visit with the medical oncologist, breast cancer patients’ resilience-related factors are assessed using a short version of the original battery of questionnaires used in the Bounce prospective pilot study. The short version was established by retraining the predictive machine learning models on the IEO data obtained in the context of the Bounce Prospective Pilot Study. Highly ranked variables were identified as predictors of 6-month mental health outcomes. After the patient fills out the questionnaire, a risk profile is generated by the DST and available to the psychologists, detailing the level of risk and the specific factors that uniquely predicted mental health for that specific patient.
During the first meeting with the IEO psychologist, the patient is given feedback on the profile of her responses to the assessment questionnaires. Patients with a low-risk profile are then contacted after 3 and 6 months for a follow-up and to complete the same questionnaires as at baseline.
Patients with a high-risk profile are assigned to two groups:
1) a group receiving conventional psychological intervention. In this group, the psychologist is blind to the DST-generated patient-specific risk profile and only knows that the patient is at risk of poor mental health; similarly, the patient knows only that she has a high risk of poor resilience and mental health;
2) a group receiving customized intervention based on the patient-specific risk profiles. With the support of the graphs generated by the DST patient-specific model, she is informed about the factors most likely to promote or thwart long-term mental health and how working on such factors can lower the risk. The psychologist then plans an intervention focused on the discussed factors.
Both groups receive a total of ten psychological consultations.
Despite the testing pilot being still ongoing, the advantage of visualizing and discussing the patient-specific profile with the patient is already apparent. Not only the model confirms what patients often describe as crucial weaknesses and strong points in their initial interview but also it helps patients to better understand their psychological condition and facilitates their engagement in the psychological intervention.
After the analysis of the patient’s profile, the psychologist discusses with her the results supported by a graph summarizing the overall risk profile. Additional graphs are presented as visual aids of the potential significance of specific predictive variables. When walked through the illustrations, patients showed a good understanding of the underlying concept and the need to work on significant predictors in order to lower the risk of poor outcome.
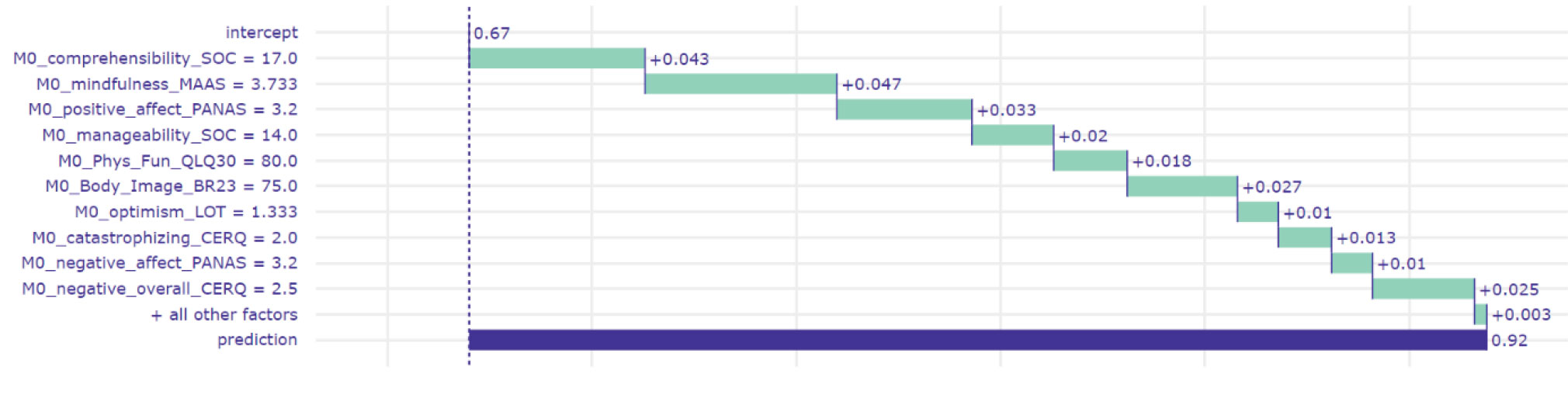
Overall profile discussed with the patient
The patient is walked through the meaning of the graph, describing the variables that emerged as most significant in predicting her long-term mental health outcome. In the example presented below, the model predicts a poor six-month outcome with a probability of 92%. Highest-ranking predictors in the model as trained and tested in the total sample of IEO patients are listed by order of diminishing importance from top to bottom of the graph. However, not all highly-ranking variables appear to contribute strongly to the predicted mental health outcome of this particular patient. Let’s consider for example physical functioning that despite in the top 5 variables, is not expected to facilitate long-term resilience even if it were to improve.
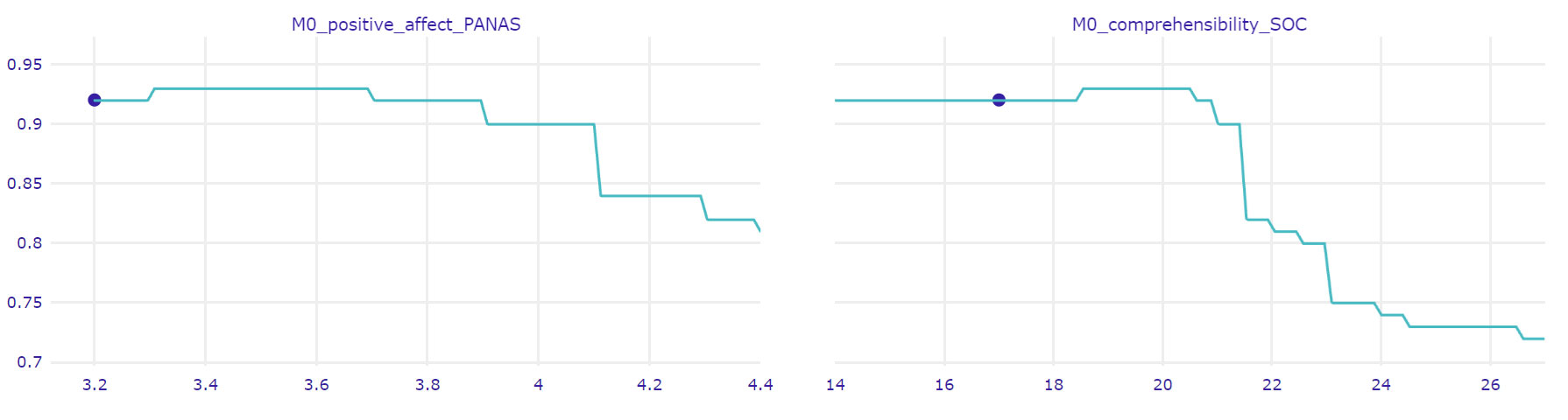
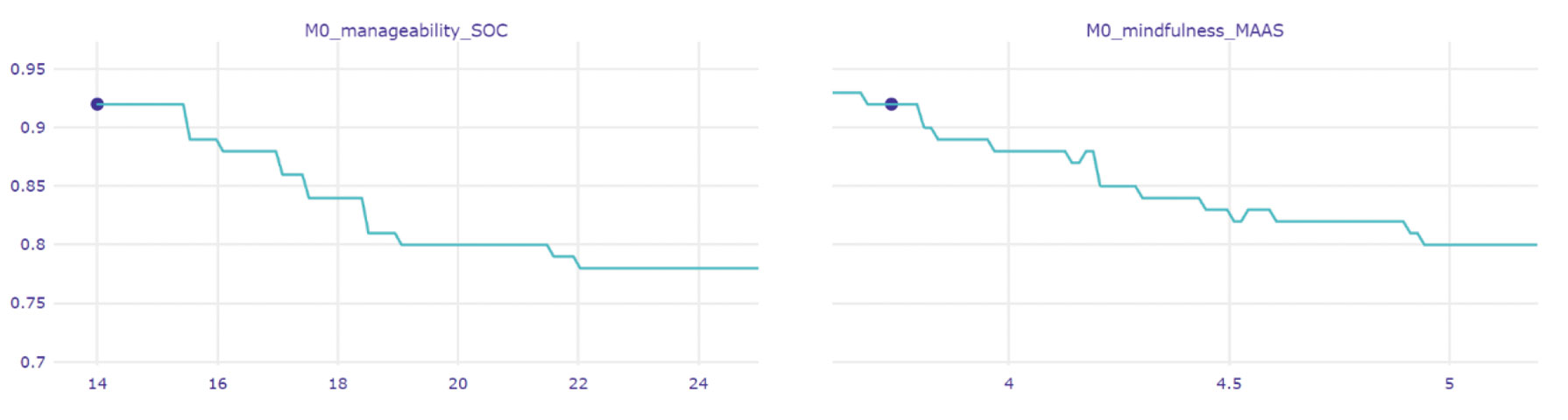
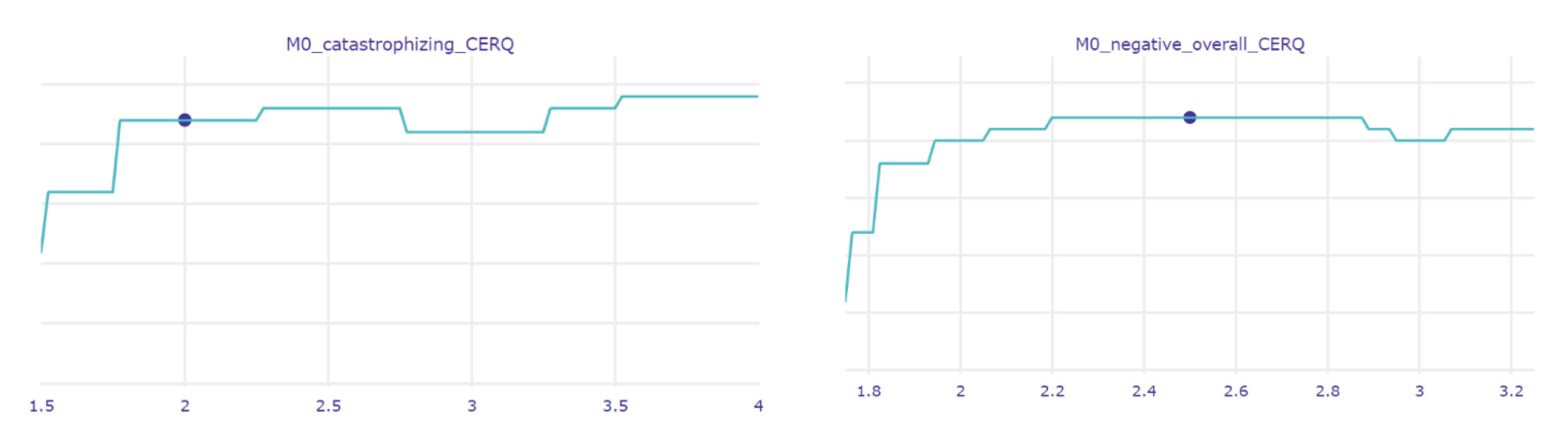
Variable-specific profiles: Focusing on optimal targets of intervention
After presenting the overall profile, the psychologist focuses on variables most likely to contribute to long-term mental health outcomes and therefore are worth working on. In this specific case, the model predicts a 10% decrease in the risk of poor mental health at 6 months, if the level of current positive affect would increase. Similarly, by increasing the level of comprehensibility (the capacity to understand the meaning of events), the risk of poor mental health at 6 months is predicted to decrease by 20%.
Additionally, the model estimated that working on Mindfulness (increasing the awareness and attention to the present moment and to what is happening and to associated feelings) and Manageability (increasing the perception of the available personal resources that respond to life demands) may further and significantly reduce the risk of an adverse mental health outcome for this patient.
A smaller but still clinically relevant change toward reducing this risk is predicted if the patient manages to moderate her tendency to catastrophize, that is to see events as worse than they are; a similar result is predicted relative to the capacity to cognitively regulate emotion.
No significant changes in mental health outcome are predicted for the remaining variables. Therefore, the psychological intervention will not focus on them and for this reason, they are not discussed with the patient.
By Ketti Mazzocco and Diana Sala, Department of Oncology and hemato-oncology, University of Milan and Applied Research, Division for Cognitive and Psychological Science, Istituto Europeo di Oncologia, Milan, Italy George Manikis, Computational Biomedicine Laboratory, Institute of Computer Science, Foundation for Research and Technology-Hellas